On this page
Osteoarthritis is a degenerative condition that affects the joints in the body. It is the most common type of arthritis and it can affect any joint in the body, but it is most common in a person’s hip or knee.
Osteoarthritis should not be confused with Rheumatoid arthritis (RA) or psoriatic arthritis which are both inflammatory driven conditions and affect the body differently.
Osteoarthritis affects the cartilage within a joint. Cartilage is a strong and smooth layer of soft tissue that coats the end of the bone that is within a joint. These characteristics of cartilage allow the bone to move with less friction in a joint. Osteoarthritis causes this cartilage to become thinner and more uneven. This means that the joint does not move as smoothly as it should.
People with osteoarthritis can experience a variety of symptoms at the affected joint. Most people will develop osteoarthritis in their joints as they get older, but this does not always cause obvious symptoms. One of the reasons that some people do not experience severe symptoms is because of a process that some professionals refer to as ‘wear and repair’.
This occurs when cells in the joint (chondrocytes) become more active because of the changes to the cartilage and the cells assist in repairing the cartilage, allowing the joint to work more normally.
Sometimes this works well. But other times, the repair process doesn’t work as it should and this can cause further changes in your joint.
Conservative treatments, like physiotherapy, aim to promote the ‘wear and repair’ process using activity modification to manage osteoarthritis symptoms. These styles of treatment can also help you to manage your symptoms.
Symptoms
Symptoms you may experience with osteoarthritis at the hip or knee:
- Joint pain – often worse with prolonged rest/movement or at the end of the day.
- Joint stiffness – often worse after rest and eases with movement.
- Joint swelling – which may cause the joint to feel hard/knobby or soft/puffy.
- Crepitus – the experience of cracking/popping sounds within a joint.
- Muscle wasting in the thigh or gluteal muscles.
- Knee specific symptoms:
- Most painful when you walk up or down gradients or stairs.
- Difficulty bending the knee through full range.
- Hip specific symptoms:
- Pain in the groin or outside of the hip.
- Difficulty putting socks/shoes on.
- Difficulty getting in or out of a car.
Causes
Our joints have the ability to repair themselves and this process is reduced by osteoarthritis.
Osteoarthritis is not as simple as wear and tear, there are many influencing factors when considering your risk of developing osteoarthritis.
The factors that increase the risk of developing osteoarthritis include:
- Age – Most common in people over the age of 45. It is not exactly known why people in this age group are more likely to develop the condition, but it may be due to bodily changes associated with weakening of muscles, weight gain, and the slowing of healing processes.
- Obesity – carrying excess weight can inflict significant stress on the body, particularly on the weight-bearing joints such as the hip or knee. Additionally, carrying excess body fat increases inflammatory processes in the body, these processes can increase the severity of osteoarthritis symptoms.
- Sedentary lifestyle – Our joints need loading to deliver essential nutrients into the cartilage. An inactive lifestyle can prevent this process and slow the repair of damaged cartilage.
- Previous trauma – Previous major injury or operations on a joint can predispose a joint to develop osteoarthritis.
- Genetic factors – if one of your family members has had osteoarthritis you may be more likely to develop it. Also, specific gene variations may affect cartilage and connective tissues
What can I do to help my symptoms?
Although there is no cure for osteoarthritis there are different treatments that you can use which may help you to control and improve your osteoarthritis symptoms.
You can access some of these treatment options at home or from your GP/occupational health service.
These treatment options include:
- Pain management
- Physical therapies / activity modification
- Lifestyle changes
- Medical management
Pain management
Pain management techniques do not usually change the disease process of osteoarthritis, but they can help to ease the symptoms of pain and stiffness. Therefore, it is advised that pain management is used alongside other treatment techniques.
Heat therapy
Applying heat to affected joints can help relax muscles, increase blood flow, and reduce stiffness, ultimately providing pain relief for a short period of time. You can apply heat using: hot water bottles (wrapped in a towel to protect your skin), wheat packs (that can be heated in the microwave), or submerging in warm water.
You should limit heat application to 15-20 minutes at a time to prevent skin irritation or overheating.
Cold therapy
Cold therapy can be very effective in reducing any new pain which is associated with sudden swelling and tenderness. You can apply cold therapy to the affected joint by applying ice or submerging the affected joint in cold water.
Ice must be used correctly otherwise ice burns can occur.
- Wet a cloth under a cold tap and then wring the cloth out until it is just damp.
- Place the damp cloth over the affected area and then place either a plastic bag of crushed ice or a packet of frozen peas on top of the cloth.
- Leave the ice pack and cloth in place for approximately 10-15 minutes and repeat 3 to 4 times a day.
Crushing the ice into small pieces allows it to mould better to the area
Do not use ice if you have circulatory problems, such as Raynaud’s disease, history of cold induced hypertension, peripheral vascular disease, allergy to cold (urticarial or joint pain) or sickle cell anaemia. If your skin is usually numb over the injured area, please speak to your physiotherapist or GP before using a cold pack / ice.
It is normal for your skin to go slightly red or pink. Remove the ice if extreme redness/pain, blistering or an increase in swelling occurs. If you experience these symptoms, please call NHS111 for further advice.
Movement
After prolonged periods of rest, simply moving your joint for 5-10 minutes through its full range of motion can ease symptoms of pain and stiffness.
It is important to recognise that it is okay to feel pain at your joint. The pain is caused by sensitised tissues around the joint and will not damage the hip/knee and it is beneficial to make a regular habit of movement.
Transcutaneous electrical nerve stimulation (TENS)
A TENS machine sends electrical pulses to your nerve endings through pads placed on your skin. It produces a tingling sensation and is thought to relieve pain by altering pain signals sent to the brain.
The research evidence on the effectiveness of TENS is mixed, but some people do find it helpful in relieving there pain for short periods.
Medication
Over the counter medications including paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs), like Ibuprofen, can be effective at controlling symptoms. You can obtain advice regarding medication from your local pharmacist orGP, but remember to read the packet and do not take over the recommended dosage.
Topical NSAIDs in the form of a cream or gel can also be used. These are applied directly to the specific area of pain. They can help reduce the pain and inflammation without some of the side effects of digesting anti-inflammatory tablets. Ibuprofen and Diclofenac gels are available over the counter at most pharmacies.
You can obtain advice regarding medication from your local pharmacist or GP, but remember to read the packet and do not take over the recommended dosage.
If you find that paracetamol or NSAIDs do not give enough pain relief, you could speak with your GP about other options for you.
Lifestyle changes
Sedentary lifestyle
A sedentary lifestyle can increase the severity of osteoarthritis symptoms. Maintaining an active lifestyle with regular exercise is crucial for managing osteoarthritis, as it helps strengthen muscles, improve joint flexibility, and reduce pain.
Avoiding prolonged periods of sitting and incorporating movement into daily routines is essential for joint health and overall well-being. This is because our joints need to be loaded to deliver essential nutrients into the cartilage. The cartilage in our joints does not have a direct blood supply, and instead uses compression to improve diffusion and ‘suck up’ nutrients from the surrounding synovial fluid a lot like a sponge.
An inactive lifestyle can prevent this process and slow the repair of damaged cartilage. Exercise and loading should be used in appropriate doses to avoid flare ups of pain, please read the section on physical therapies for more information.
Weight loss and diet
The clearest link between diet and osteoarthritis is related to body fat. Losing even a small amount of body fat can make a big difference to your symptoms. The best way of losing weight is by following a healthy, balanced diet. Cut down on the number of calories you get from high-fat and sugary foods, but make sure that you’re including all the key food groups in your diet and not missing out on essential nutrients.
Gradually increasing the amount of physical activity you do can also help with weight loss.
Physical therapies
Many people worry that exercising will increase their pain and cause further damage to their joints, in reality regular exercise is strongly recommended in the management of osteoarthritis and there are many proven benefits. Whilst resting painful joints may improve the pain at first, too much rest can increase stiffness and pain.
Physical activity can:
- Help you to lose excess body fat.
- Maintain and build muscle that protects and supports joints.
- Help to control pain.
- Improve mood and reduce stress (which is associated with reducing pain)
You shouldn’t be afraid to use your joints. If pain makes it difficult to get started with exercise, you could try taking a painkiller such as paracetamol beforehand. And if you feel you’ve overdone things a bit, try applying warmth to the painful joint or if it’s swollen, applying an ice pack may help.
The key to building up your physical activity is to find something you enjoy. That way you’ll be much more likely to keep it up. An easy way to become more active is to incorporate exercises into your everyday life – such as doing some stretches while waiting for the kettle to boil or opting to use the stairs over the lift.
There are three types of exercise that you should try.
Exercise for hip and knee
Cycling

- Cycling is a great exercise for both knee and hip osteoarthritis. It can help to strengthen multiple muscles around your hip and knee.
- Cycling can be completed on both the conventional push bike and a static bike that you may find in the gym.
- When setting up your bike or static bike ensure that your knee is nearly straight when your foot is at the bottom of the crank (see photos).
- Initially you should complete 5 to 10 minutes on the bike at an intensity that you can tolerate. You should aim for this exercise to be difficult for your breathing and fatiguing for your muscles.
- To progress your cycling increase your weekly volume (measured in time/distance) or intensity by no more than 10% per week to avoid over training and flare-ups of osteoarthritis symptoms.
Exercise 1a: Glute bridge
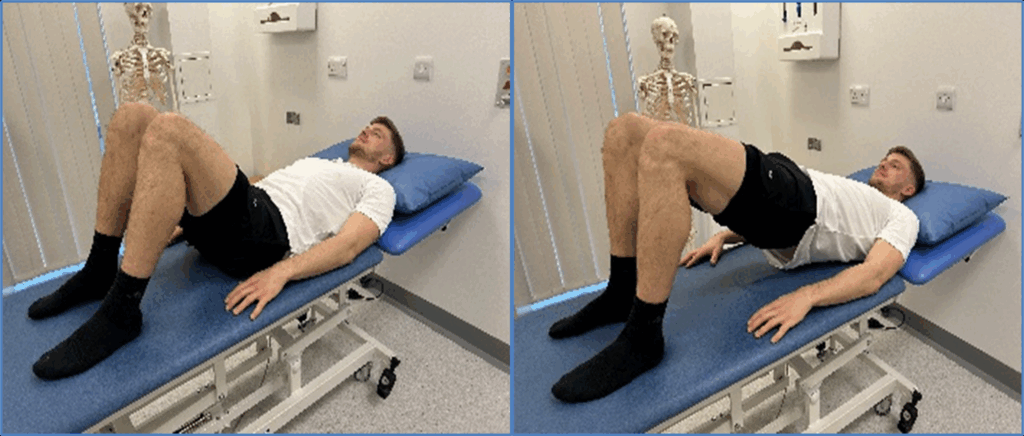
Exercise 1a: Glute bridge
- Lay on your back with your hands by your sides and both of your knees bent at a 90-degree angle if possible.
- Lift your hips off the floor and push your hips towards the ceiling.
- Focus on keeping your back straight and pause for 1-3 seconds.
- Return to starting position and repeat.
Tips
- Exhale as you lift up and inhale as you return to starting position.
- This exercise should be felt in your buttocks, targeting your gluteal muscles. At the start of the movement push your lower back into the bed to help achieve this activation.
- If this exercise is too difficult attempt the one below instead.
Exercise 1b: Pelvic tilts
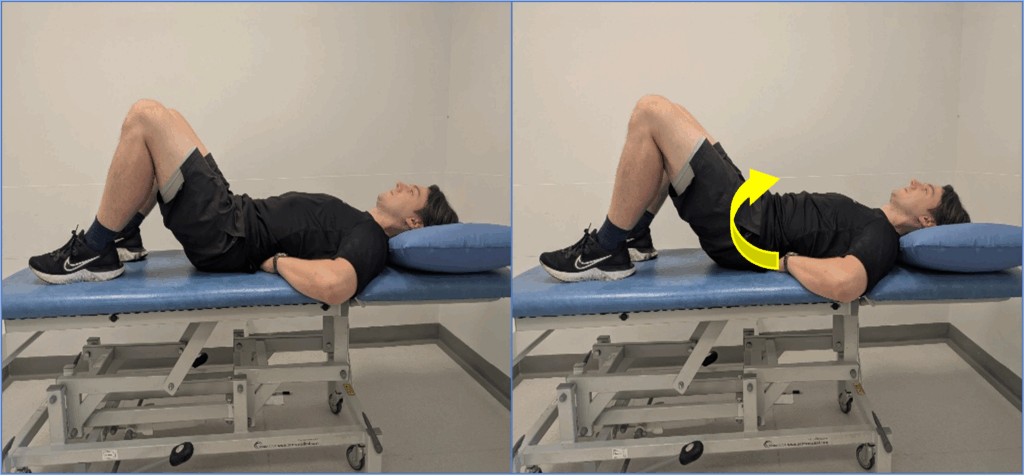
Exercise 1b: Pelvic tilts
- Lay on your back with your hands by your sides and both of your knees bent at a 90-degree angle if possible.
- Squeeze the muscles in your bum to roll your hips forwards and push your lower back into the floor.
- Focus on keeping your back straight and pause for 1-3 seconds.
- Return to starting position and repeat.
Tips
- Exhale as you lift up and inhale as you return to starting position.
- This exercise should be felt in your buttocks, targeting your gluteal muscles.
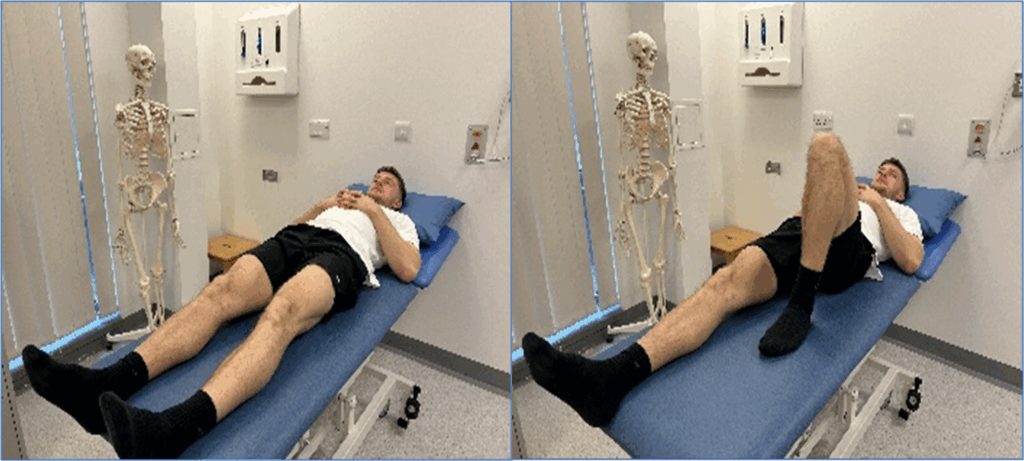
Exercise 2a: Straight leg raise
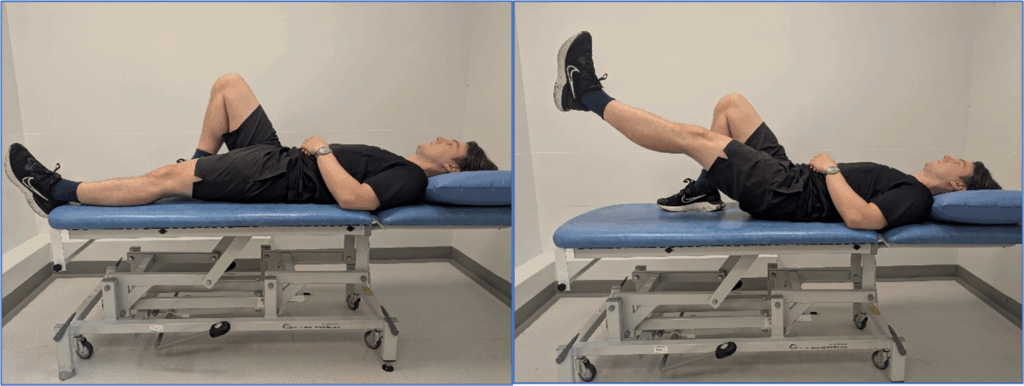
Exercise 2a: Straight leg raise
- Lay flat on your back, with your hands rested by your side or on your stomach. Bend one of your knees to as close to 90 degrees as possible (as seen in the photo).
- Lift the straight leg up towards the ceiling as far as you can tolerate whilst keeping your leg straight.
- Hold the leg up for 1-3 seconds then slowly lower back down.
Tips
- Try to focus on keeping your mid to lower back in contact with the floor during repetitions.
- You should feel this exercise across the front of your hip and thigh, targeting your hip flexor and quadriceps muscles.
- If this exercise is too difficult attempt the one below instead.
Exercise 2b: Lying knee flexion
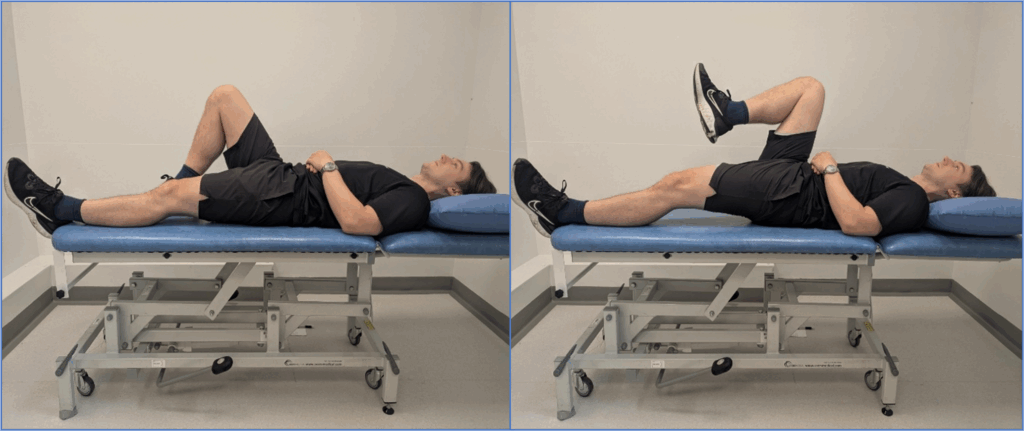
Exercise 2b: Lying knee flexion
- Lay flat on your back, with your hands rested by your side or on your stomach. Bend one of your knees to as close to 90 degrees as possible (as seen in the photo).
- With the knee that is bent, bring the knee into towards your chest (without using your hands) as far as you can tolerate.
- Hold the knee up for 1-3 seconds then slowly lower back down.
Tips
- Try to focus on keeping your mid to lower back in contact with the floor during repetitions.
- You should feel this exercise across the front of your hip, targeting your hip flexor.
Exercise 3a – Side lying hip abduction
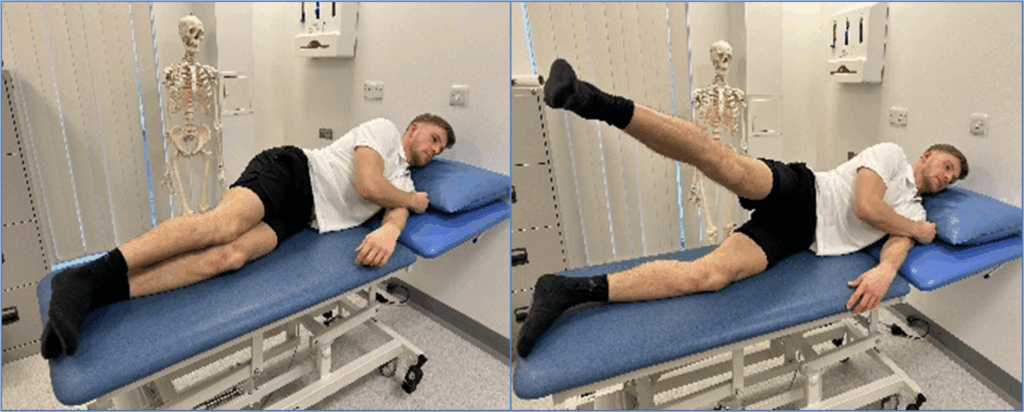
Exercise 3a – Side lying hip abduction
- Lay on your side with your legs fully extended and stacked on top of each other.
- Keep your hips & shoulders aligned.
- Lift your top leg straight up to around 45 degrees if possible.
- Hold for 1-3 seconds then slowly lower down.
Tips
- You should feel this exercise on the side of your hip, targeting your gluteal muscles which play a key role in postural stability.
- Breathe out as you lift up and in as you lower.
- Try to keep your pelvis stabilised during each rep, prevent it from rolling backward.
- If this exercise is too difficult attempt the one below instead.
Exercise 3b – Standing hip abduction
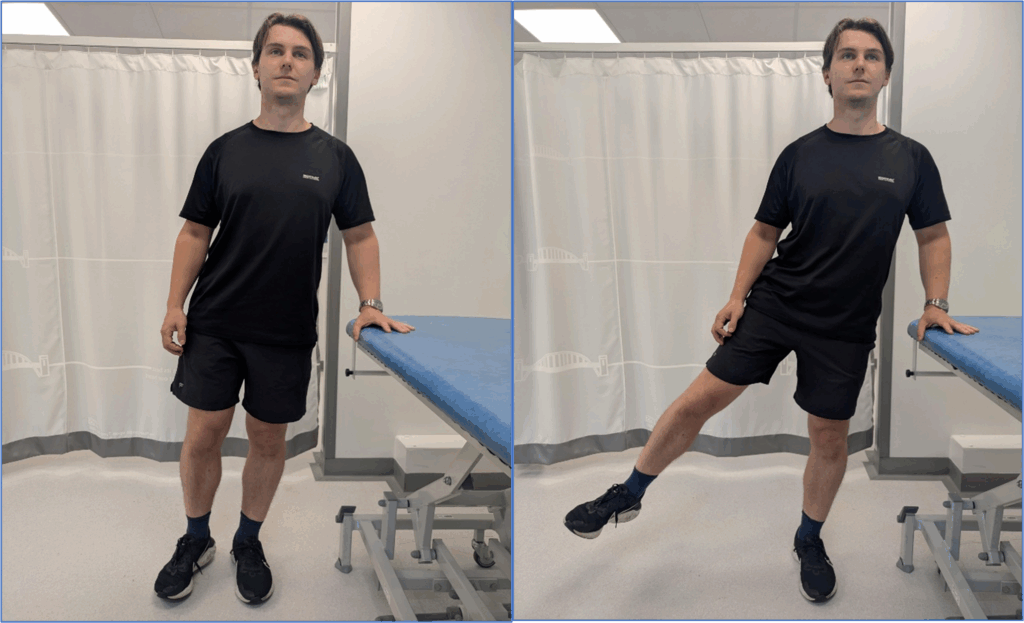
Exercise 3b – Standing hip abduction
- Stand in an upright position with a chair or table besides you for you to hold onto for support.
- Was keeping the foot closest to the chair or table planted to the floor. Lift the other leg out to your side in a slow and controlled motion (as seen in the photos).
- Keep lifting your leg until you can’t any further at hold for 1-3 seconds then slowly lower down.
Tips
- You should feel this exercise on the side of your hip, targeting your gluteal muscles which play a key role in postural stability.
- Breathe out as you lift up and in as you lower.
- Try to keep your pelvis stable and avoid twisting during this exercise to avoid compensation from different muscles.
Exercise 4 – Clams
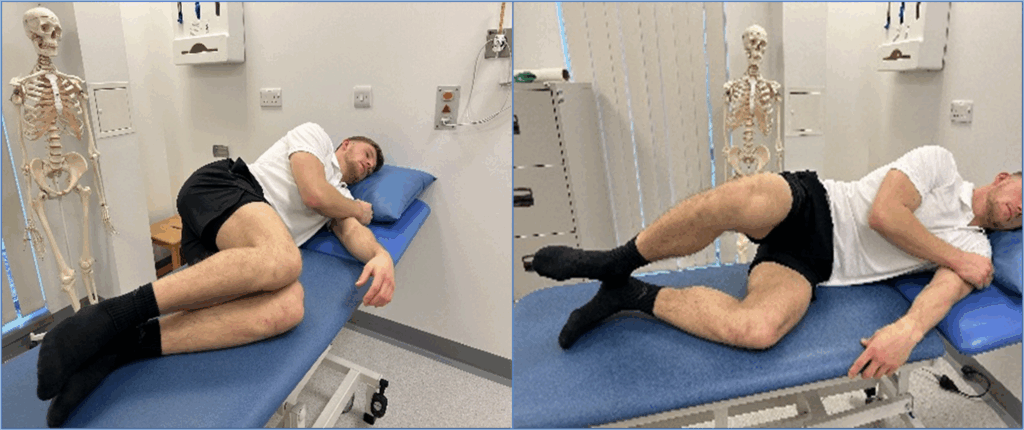
Exercise 4 – Clams
- Lay on your side, with your knees bent at 45 degrees, your feet/heels will remain in contact with each other throughout.
- Lift your top knee, whilst focusing on keeping your pelvis stable.
- Hold for 1-3 seconds then slowly lower back down.
Tips
- Try to keep your pelvis stabilised during each rep, prevent it from rolling backward.
- Breathe out as you lift up and in as you lower.
Exercises focusing on the knee
Exercise 1: Knee flexion
Exercise 1: Knee flexion
- Lay flat on your back with your hands resting on your stomach or down by your side.
- Bend one leg at a time, sliding your heel upward toward your buttock.
- Flex your knee maximally.
- Slowly lower your leg back down to starting position.
Tips
Try to focus on keeping your mid to lower back in contact with the floor during repetitions.
Exercise 2a: Mini squat (chair for safety).
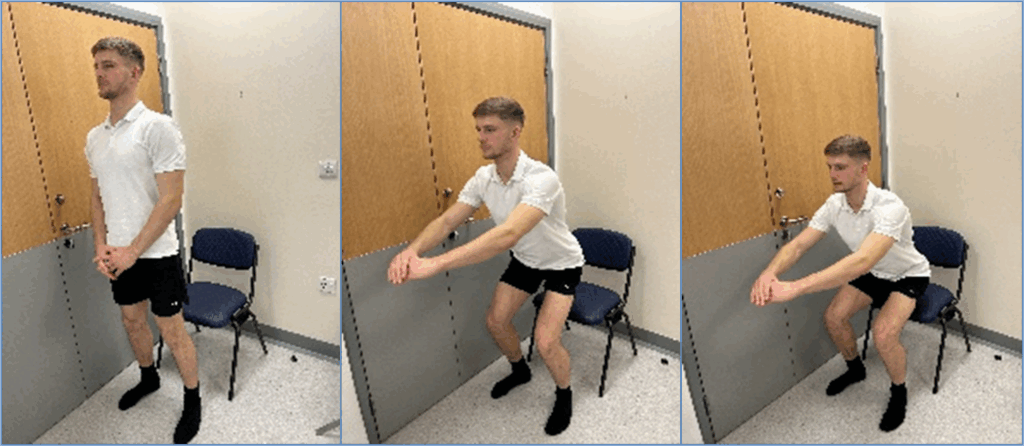
Exercise 2a: Mini squat (chair for safety).
- Begin standing in front of a chair, feet shoulder-width apart and in a comfortable direction for you.
- Slowly lower yourself down whilst squeezing you core muscles and keeping your chest up.
- Keep lowering yourself until your knees are at a 90 degree bend.
- Then press through your heels to stand back up to the starting position.
Tips
- Attempt to align knees with the direction of your feet.
- Try to evenly distribute your weight throughout.
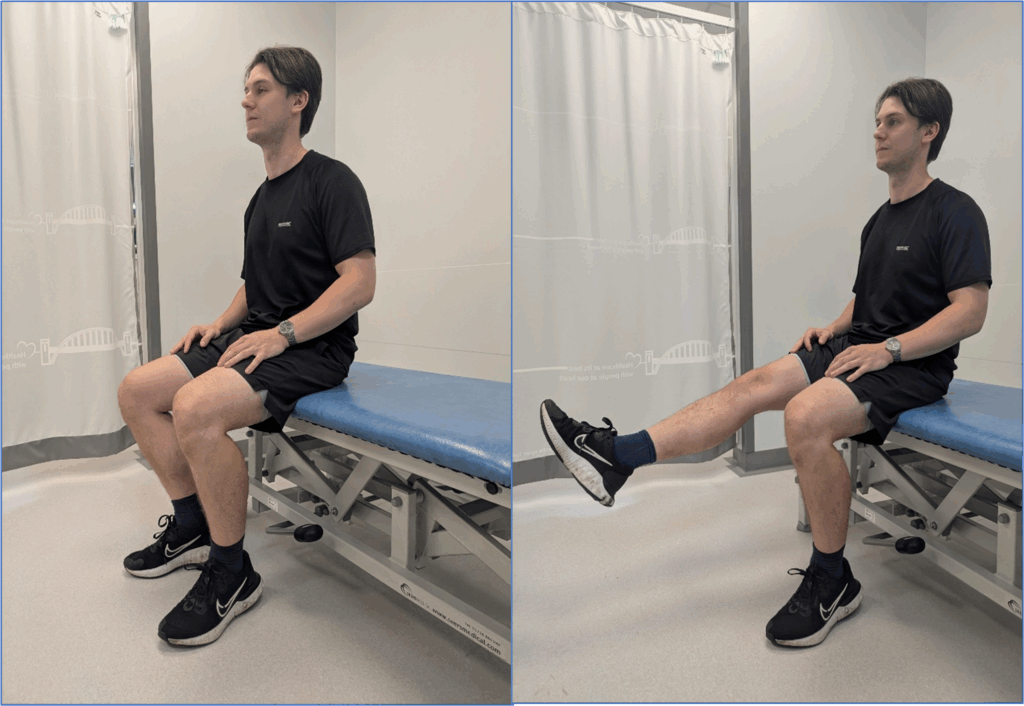
Exercise 2b: Sit to stand
Exercise 2b: Sit to stand
- Begin sitting on the edge of a chair, and with your feet shoulder-width apart and in a comfortable direction for you.
- Bring your head forwards so that your nose is over your toes.
- Push through your feet to stand up in a controlled movement, focusing on a steady stand. Try to avoid using your hands if you can tolerate this.
- Slowly lower yourself down whilst squeezing you core muscles and keeping your chest up until you sit back onto the chair.
Tips
- Focus on control of the movement – quality over quantity!
- Attempt to align knees with the direction of your feet.
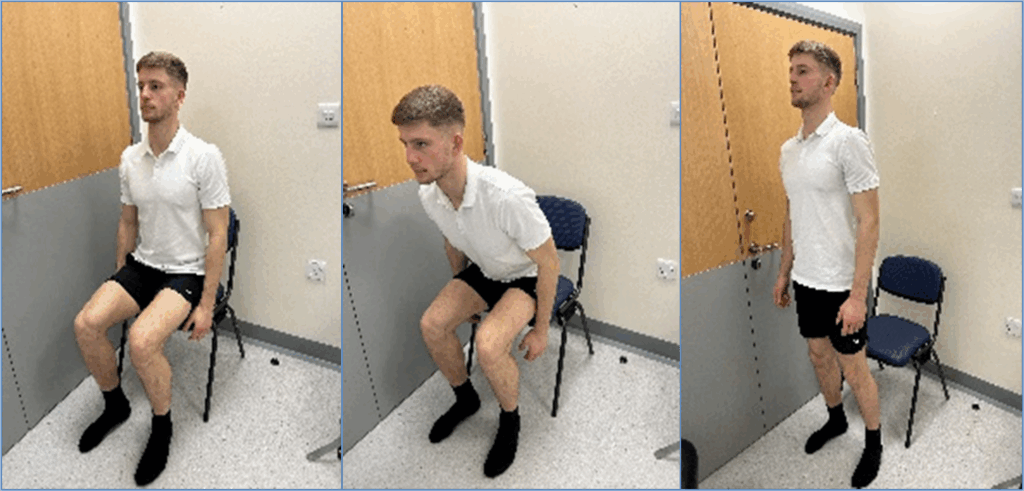
Exercise 3: Seated knee extension
Exercise 3: Seated knee extension
- Sit on a stable surface. You will need a leg length’s worth of open space in front of you.
- Straighten one leg out in front of you as far as you can tolerate.
- Hold in the end position for 1-10sec depending on your tolerance.
- The slowly bend the leg back to the starting position.
Tips
You should feel this exercise on the front of your thigh, targeting your quadriceps muscles.
Exercise 4: Step up

Exercise 4: Step up
- Stand just before a sturdy step, flex at the hip & flex your knee to clear the step with your foot.
- Engaging your core stability muscles, safely plant your foot on the step.
- Push through your leading leg to bring your trailing leg to meet.
- Once up on the step, reverse this process to safely return to starting position.
Tips
Focus on the leading leg doing the work by not allowing excessive force from the trailing leg to step up.
If you can perform these exercises comfortably more advanced exercises can be found at:
Invasive treatment options
If your OA symptoms continue to significantly impact your function and quality of life following a prolonged trial of the above treatments, then your GP may consider you for further intervention.
Corticosteroid Injections
A corticosteroid injection may be provided to help relieve pain and inflammation. The corticosteroid injection won’t cure osteoarthritis and the goal of this injection is often to provide short term improvement of symptoms to enhance adherence and outcomes with physical therapies.
Following a corticosteroid injection, symptoms typically begin to improve 1-3 weeks after the injection, and this may last several weeks to several months. Repeated use of injections is evidenced to weaken the soft tissues in and around the joint and this may lead to advancement of symptoms or other musculoskeletal issues. This is something your GP/physio will discuss further with you upon their consultation.
Surgery
Surgical intervention will likely only be considered if all conservative treatments fail.
A total hip or knee replacement (arthroplasty) has the potential to improve pain and function. A course of rehabilitation is required after a joint replacement to optimise recovery and function of the joint. A successful surgery and rehabilitation can improve osteoarthritic symptoms, however, there are risks to surgery, which would be discussed with the orthopaedic team upon consultation.
What about work?
Maintaining all normal activities (including work duties) will improve your chance of maintaining or gaining optimal function. Keeping your joints moving will help you to keep your ‘work fitness’ and minimise further changes to the cartilage in your joints.
You do not have to be pain free to remain at work.
It may be appropriate to do focus on temporary lighter or modified duties. This is something that can be discussed with your line manager initially. If further support is needed your line manager can complete a referral to the occupational health service to help identify more specific role modifications
What should I do if I am still experiencing problems?
If you are unable to agree on restricted roles with you manager or you are still having problems the occupational health service may be able to help.
The occupational health service can advise you on how to bridge the gap to help you return to normal activities.
You can also access the occupational health physiotherapy team by:
Self-referral
The occupational health physiotherapy team can assist in the management of musculoskeletal problems that affect your ability to work.
Management referral
If you feel your symptoms are having a significant effect on your ability to carry out your role, discuss this with your manager and request a referral to the occupational health service.
Contact
Physiotherapy team
Ground Floor
Regent Centre
Regent farm road
Gosforth
NE3 3HD