This important information will be of use to you throughout your treatment. – Please keep it for reference. If you have any further queries or require any additional information please do not hesitate to contact the nursing team on 0191 2138213.
On this page
- What is egg or embryo freezing?
- Why might I want to freeze my eggs or embryos?
- How long can I store my eggs or embryos for?
- Will I have to pay for freezing and storage?
- Preparation for treatment:
- Prescriptions
- Appointments
- Medication and injections
- What happens during the treatment?
- Risks of treatment
- Follow-up
- Counselling Service
- Support Groups
- Patient feedback
What is egg or embryo freezing?
Egg freezing is a relatively new method that involves storing mature oocytes (“eggs”) that have been collected following a course of treatment. Single women or women in relationships can store their eggs.
Embryo freezing is the storage of eggs that have been fertilised and developed in the laboratory for 5-6 days to develop into blastocysts. Embryo freezing is only considered for couples where the male partner can provide a sperm sample. Any future use of the embryos would have to be agreed by both partners. This means that if your relationship was to end your ex-partner would have to agree to you using the embryos to create a pregnancy and that he would be the legal father of any child born from the embryos. If he withdraws his consent for you to use the embryos you would not be able to proceed with using the embryos. It is very important that you carefully consider this before deciding if egg or embryo storage is best for you.
Why might I want to freeze my eggs or embryos?
There are a number of reasons why women might want to freeze their eggs or embryos. Some of these include:
- Women of reproductive age (including adolescent girls), who are preparing for medical treatment for cancer or other conditions that are likely to make them infertile.
- Young women at high risk of premature ovarian insufficiency.
- Women undergoing mitochondrial donation.
- Women who want to delay childbearing.
How long can I store my eggs or embryos for?
Eggs and embryos can be stored for up to 55 years. The need to continue storage must be reviewed at least every 10 years.
Will I have to pay for freezing and storage?
In most situations funding is available for egg or embryo storage but in some cases e.g. delaying childbearing that is not the case and you would need to pay for all of the process. Even if the original egg or embryo freezing treatment has been NHS funded it is possible that if your situation changes you may have to pay for ongoing storage costs. In addition funding for fertility preservation does not mean that the use of stored eggs or embryos will be funded at a later stage since this is dependent on commissioning available for fertility treatment at the time you seek future treatment. Please ask if you want to know more about this. We can advise about how funding stands now but cannot give definite advice about future commissioning.
Preparation for treatment:
Ovarian reserve: We will perform a blood test and an internal (vaginal) ultrasound scan to assess your ovaries. This helps us to roughly estimate, and advise you, of the potential success of retrieving a reasonable number of oocytes. It also helps us decide on the dose of drugs that we will use. If your ovarian reserve is reduced it may not be appropriate to consider oocyte storage.
Folic Acid: All women who are trying to conceive are advised to take Folic Acid 400mcgms daily to reduce the risk of a baby born with spina bifida. It is often cheaper to buy this over the counter at a chemist than on prescription. In some situations – if there is a personal or family history of spina bifida or when the woman is taking some medications e.g. some antiepileptic drugs it is advisable to take a higher dose. The known benefit is to the developing child (fetus) however we would suggest that you take folic acid prior to egg storage also.
Weight: Being overweight has serious health implications and can cause complications during pregnancy. If you are overweight we will discuss this with you during your consultation and advise you to lose weight. We may defer your treatment until you have lost weight. It is important that you maintain your weight loss throughout the time you are having treatment.
Smoking: Research suggests that women who smoke are less likely to conceive following fertility treatment. There are well known health benefits in stopping smoking. It is therefore strongly recommended to stop smoking before embarking on fertility treatment. If you would like help to stop smoking please speak to the nurses who can offer you advice or telephone the NHS Smoking Helpline 0300 1231044.
Alcohol: The Department of Health advises that women trying to conceive should avoid drinking alcohol. If they do choose to drink, they should not drink more than one to two units of alcohol once or twice a week and should not get drunk.
Cervical smears: It is advised that you ensure that your smears are up to date prior to commencing fertility treatment so that any further assessment or treatment can be undertaken before any potential pregnancy.
Genetic problems: Please inform us if you aware of any conditions or illnesses that exist in your family. This will allow us to investigate any risks to you or any child that you may have and ensure that you receive appropriate advice and counselling. We may refer you to a genetics specialist who can offer you specialist advice and arrange further investigations.
Infections: Sexually transmitted diseases caught at any time may create further problems when trying to conceive. If you are worried about this at any time we encourage you to visit your local genitourinary medicine clinic.
Travel Abroad: Travelling abroad may carry health risks for pregnant women or women who plan to get pregnant (e.g. Zika virus and Ebola). We advise any patients (male or female) who have recently travelled or are planning to travel abroad to refer to the department of health guidelines about any risks relating to pregnancy. If you are unsure about this please discuss with the clinic staff.
To minimise the risk of Zika Virus transmission, female travellers (symptomatic or asymptomatic) should not try to conceive naturally, donate/store gametes or proceed with fertility treatment for 8 weeks. To minimise the risk of Ebola transmission, egg donors and female fertility patients should defer from treatment or donation for 6 months after leaving an area affected at the time by an Ebola outbreak.
Covid-19 vaccination: People of reproductive age are advised to have the vaccine when they receive their invitation for vaccination. This includes those who are trying to have a baby as well as those who are thinking about having a baby, whether that is in the near future or in a few years’ time. There is absolutely no evidence, and no theoretical reason, that any of the vaccines can affect the fertility of women or men.
Blood Tests: Prior to treatment a series of standard blood tests are taken:
Full blood count – this allows us to check that you are not anaemic. An abnormality may warrant further investigation or simply a recommendation to take iron supplements.
AMH – this allows us to estimate how well your ovaries will respond to stimulation treatment. The result may have a bearing on how we treat you and also your chances of success – the result will be discussed in the clinic.
Screening for HIV, Hepatitis B and Hepatitis C. Unfortunately we are currently unable to store eggs for patients that test positive for these blood borne viruses. The screening tests for these infections will occasionally result in an equivocal or false positive result. A diagnosis of infection is not made until a formal diagnostic test confirms it.
You may require further blood tests for assessment of any fertility or medical problems prior to treatment. These tests will be explained to you as they are undertaken.
Prescriptions
Private patients will be issued a private prescription and drugs will be charged on this basis. You will be charged for the drugs when they are dispensed by the pharmacy. NHS patients will be issued a NHS prescription and will have to pay the usual NHS prescription charges.
Both private and NHS prescriptions may be obtained at the Royal Victoria Infirmary hospital pharmacy (Lloyds – New Victoria Wing). Prescriptions must be collected within one month of issue. You can collect your needles and syringes from the Fertility Centre.
Please ensure that you have collected your drugs before you are due to start the treatment cycle. Check the expiry dates and storage instructions on each drug as some items may need to be stored in the fridge.
Consent and Photo identification
It is a regulatory requirement that we have a copy of both you and your partner’s (if storing embryos) photographic identification prior to treatment. This will be uploaded to Fertility Consent, an online platform which provides patient information and relevant consent forms. These need completing before starting treatment.
Appointments
We understand that getting time off work for appointments can be difficult. It may be helpful to discuss what is happening with your employer. We can provide proof of your appointments if necessary. Please remember that the treatment dates are only an estimate of how your body will respond to the drugs. This means that we may have to alter the treatment dates in response to the scan results to ensure that you have the best chance of a successful egg collection. This can sometimes be at very short notice.
Medication and injections
We use several different medication protocols to prepare patients for egg collection. Each protocol is tailored to the specific needs of the patient and will be fully explained to you before you start any medications. Each protocol may consist of the following:
Controlling your Natural Cycle: You may be asked take injections of Buserelin Acetate (Supercur) that will temporarily switch off your natural cycle and allow us control of your cycle. Alternatively we may use the timings of your natural cycle to allow us to progress with treatment.
Stimulating your ovaries (boosting egg supply): You will be asked to take follicle stimulating hormone injections (e.g. Menopur or Rekovelle) to stimulate your ovaries to produce eggs. Follicles are tiny fluid filled sacs that grow on the ovary and contain the eggs. In your normal monthly cycle, only one egg is produced. Following treatment with hormone injections more will be available for collection.
Controlling ovulation (release of eggs): You may be asked to take a drug called Cetrotide. Cetrotide blocks the effects of a hormone called gonadotrophin releasing hormone that controls the secretion of another hormone called luteinising hormone which induces ovulation. Cetrotide will prevent premature ovulation.
Monitoring egg growth: We will watch the number of eggs in you ovaries by doing a series of scans. We will count the number of follicles developing in the ovaries and measure them. When the follicles reach about 16mm, we would expect the eggs inside to be ready to respond to the next stage of treatment, the trigger injection.
Sometimes the ovaries respond inadequately to the drugs and produce very few, if any, follicles. A decision will be made as to whether the treatment cycle is to be continued, in spite of the very poor chance of success or cancelled. If the latter option is chosen you will be offered a consultation to see a doctor during which other treatment options (if there are any) will be discussed. Occasionally a blood test will be needed to confirm the scan results.
Injections
We will teach you (or a partner or family member or friend) to administer the injections. It is simple to learn, and much easier than having to visit your doctor every day. If you choose not to do your own injections and wish to go to your GP, you must make arrangements for this yourself, remembering that some injections have to be given at weekends or evenings.
Unfortunately, we cannot arrange for injections to be given in the unit as we do not have the staff available. We will also supply you with the needles and syringes you need. We will provide a special container for the disposal of used needles and glass. Please do not put these in your household rubbish.
Needles and syringes
You can collect needles and syringes and a sharps box from the Newcastle Fertility Centre. Please return the sharps box and any unused items to the centre for safe disposal.
What happens during the treatment?
Egg and embryo freezing involves the following steps:
- Suppressing your natural cycle
- Boosting your egg supply
- Monitoring your progress and maturing your eggs
- Collecting the eggs
- Fertilising the eggs (IVF or ICSI) (embryo freezing only)
- Freezing the embryos.
There are two different treatment protocols; the long protocol and the antagonist protocol.. Most women will follow the long agonist protocol. Women who need urgent egg or embryo freezing or women with a very high ovarian reserve who have a higher than average risk of developing OHSS will follow the antagonist protocol. This is because the antagonist protocol can reduce their chance of developing OHSS. We will explain your protocol and our reasons for choosing it before you start the medication.
Long protocol
The long protocol treatment cycle will take approximately five weeks from starting the first drug until the egg collection, although this may vary depending on your response to the medications.
Antagonist protocol
The antagonist treatment cycle can take approximately 2-3 weeks from initial scan until the egg collection although this can vary depending on your response to the medications.
Step 1 – Suppressing your natural cycle (long protocol only)
Buserelin Acetate (Suprecur) injections will temporarily ‘switch off’ your natural cycle to allow us to control the timing of your treatment cycle. This is perfectly safe to do and there is no evidence to suggest it affects your future fertility. We will give you a programme before you commence your treatment cycle that informs you when to start your injections.
Step 2 – Boosting your egg supply
Medication is used to encourage the ovaries to produce more eggs than usual.
Follicle Stimulating Hormone (FSH) injections stimulate the ovaries to produce eggs. Stimulation injections are administered daily under the skin (subcutaneous). Follicles are tiny fluid filled sacs that grow on the ovary and contain the eggs. In your normal monthly cycle, only one egg is produced. To increase the chances of pregnancy with IVF treatment, we need several eggs. The average number of eggs retrieved is eight.
When do I start taking the Menopur or Rekovelle injections?
The expected date for you to start the injections is given on your treatment programme. The date will be confirmed once we are sure that the Buserelin has been effective. This date is not set in stone, and it is normal for your cycle not to go exactly according to your programme.
Menopur
Menopur is a form of Follicle Stimulating Hormone (FSH) used to stimulate the ovaries to produce eggs.
Menopur is a daily injection and must be taken at the same time every day (preferably in the morning). It can be used both in the long protocol and the antagonist protocol. It should be kept in a cool, dry place and away from direct heat or sunlight. We will ensure you know how to do the Menopur injections when you are ready to commence them. You will be instructed when to start and stop taking the Menopur injections.
Rekovelle
Rekovelle injections are only used as part of the antagonist cycle. It is in the form of an injectable pen and must be kept in the fridge. You must take this injection at the same time every day.
Rekovelle is a form of Follicle Stimulating Hormone (FSH) and the dose is decided based on your weight and AMH levels. This allows us to find a balance between stimulating the ovaries as best we can whilst preventing over stimulation of the ovaries.
It is fine to have sexual intercourse during treatment however you must use barrier contraception, such as condoms, between starting the FSH injections and the egg collection.
Cetrotide injections (antagonist protocol only)
Cetrotide (cetrorelix acetate) is only used as part of the antagonist cycle and must be kept in the fridge. It is used to suppress ovulation when the follicles have started to develop.
You will be advised when to start the Cetrotide injections. You must take this injection at the same time every day (preferably in the morning). We will instruct you on when to start and stop this medication.
Step 3 – Monitoring your progress and maturing your eggs
We watch the number of eggs growing in your ovaries by doing a series of internal scans. The first scan is usually a week after you start the injections. Your treatment programme will tell you when to attend for a scan however we will confirm and book the scan in with you.
The egg is microscopic in size and cannot be seen, but it grows in a small cyst or follicle, which shows on the scan as a black shadow. The follicle gets bigger as the egg grows. We will count the number of follicles developing in the ovaries, and measure them. If you are on the antagonist protocol, you will start another injection called Cetrotide. When the follicles reach about 16mm in size, we would expect the egg inside to be ready to respond for the next stage of treatment, the trigger injection.
Sometimes the ovaries respond inadequately to the drugs and produce very few, if any, follicles. A decision will be made as to whether the treatment cycle is to be continued, in spite of the very poor chance of success or cancelled. If the latter option is chosen you will be offered a consultation to see a doctor during which other treatment options (if there are any) will be discussed. Occasionally a blood test will be needed to confirm the scan results.
Maturing the eggs
You will be asked to take an injection to mature the eggs, this is sometimes referred to as the trigger injection. It is carefully timed to your egg collection and is usually given in the evening 2 days before egg collection. You will be told when exactly to take the injection after you have the last scan before egg collection.
There are two types of trigger injection. One is for patients on the agonist protocol (ovitrelle) and one is for people on the antagonist protocol (buserelin). The decision making process regarding this is explained later in this document, in the OHSS section. We will teach you how to do your prescribed trigger injection..
If you are freezing embryos your partner should ejaculate on the day you have your trigger injection and not again until he produces the sample for egg collection.
Can I have sex?
It is fine to have sex during treatment however you must use barrier contraception, such as condoms, between starting FSH and embryo transfer.
Step 4 – Collecting the eggs
Egg collection
The eggs are collected by using a transvaginal ultrasound scan, just like the ones you have had during the last step. A thin needle is passed along the ultrasound scan machine into the ovaries, via the vagina, to remove the eggs.
The procedure is done under sedation to ensure you are comfortable throughout. You will be offered the option of a pre medication, called Lorazepam. This is two tablets, one for the night before and one for the morning of procedure to help with nerves if you feel you will be nervous. This is perfectly safe with treatment.
When a decision is made to proceed to egg retrieval you will be given an admission form and instructions regarding your medicines. Please read this carefully because it will tell you when and where to come and what to bring with you.
If you are a single person seeking treatment you might want a friend or relative to accompany you on the day of egg retrieval. If you are attending alone you must arrange for someone to collect you from the recovery area after the egg retrieval and escort you home. You must have someone to stay with you overnight.
What happens when I am admitted?
On admission to the recovery ward, one of our fertility nurses will perform some vital observations including your temperature and blood pressure. You will need to change into a theatre gown. The nurse sedationist and operator will see you to discuss the procedure and answer any of your questions. A small needle will be used to introduce a plastic tube into a vein in your hand or arm. This is called a cannula and is how the medication will be administered to you during the procedure.
Partners or friends/relatives are welcome to stay in the unit but we will ask them to sit in the waiting room or leave the clinic once you go into theatre for the procedure. They can join you again when the egg retrieval is finished and you have recovered from the sedation. This is usually 90 minutes from the start of the egg retrieval.
What medication will I be given?
The nurse sedationist will give you two drugs through the cannula in your arm. The first drug is a pain killer (Fentanyl) and the second is a sedative (Midazolam) to make you feel calm and relaxed. You will not be asleep during the procedure but a common side effect of the sedation is that you may not remember the procedure. Some women may need further pain relief such as Entenox gas or IV Paracetemol. We will discuss this with you if needed.
You can also choose to have a pre medication (Lorazepam) the night before and the morning of the procedure if you are feeling anxious.
If you have any worries or concerns or would just like to talk to the nurse sedationists, you can contact them via the unit phone number. We have the facility to play your MP3 or IPOD if you would like to listen to some music during the egg collection.
How are the eggs collected?
Your legs will be put in special supports and you will then have an internal examination and scan. A very fine needle is inserted through your vagina and into the ovary. This is uncomfortable for just a few moments. We can then drain the fluid from each follicle. The fluid is passed to the embryologist in the next room who will identify and count the eggs and place them in an incubator compartment that is clearly labelled with your name. The procedure is repeated on the other ovary. The whole procedure lasts for about 10 minutes depending on how many follicles you have grown. We expect to obtain eggs from approximately 70% of follicles. Occasionally the egg recovery rate may be much lower than this as it is not guaranteed that each follicle contains an egg. On rare occasions no eggs are found in either ovary.
What happens after the eggs have been collected?
You will be taken back to your bed in the recovery area on a trolley. You will feel drowsy following the procedure therefore we encourage you to sleep for the first hour. It takes at least an hour for the initial effects of the drugs to wear off so you must stay on our recovery area for that time.
The sedation drugs may leave you with a dry mouth, you may feel drowsy and you may have the inability to perform complex tasks. As it takes 24 hours for the sedation drugs to wear off completely you should rest at home for this period of time. You must have someone with you at all times until the following morning.
You should not drink alcohol, use electrical equipment or machinery or drive for 24 hours.
You should also not sign any legal documents during this time.
If you live more than 40 minutes away from access to emergency care we advise you to stay locally.
Once you are awake and feeling well enough to go home the embryologist will visit you to advise how many eggs were retrieved. If we are storing eggs we will assess the eggs for suitability for storage and let you know as soon as possible how many were successfully stored. This could be on the day of egg collection or the day after. If we are storing embryos the embryologist will discuss the number of eggs available for insemination, the results of the semen analysis and confirm if they need to do IVF or ICSI to inseminate the eggs.
What will happen after I go home?
It is normal to have some abdominal discomfort. You can take two Paracetamol tablets every 4 hours but be careful not to take any more than 8 tablets in 24 hours. If the pain is severe and persistent or you are vomiting please telephone the centre. Brown vaginal spotting or discharge is not uncommon and will usually settle after approximately 48 hours.
We advise you to have a light meal that evening as you may feel quite bloated.
Sperm preparation
If you are storing embryos a semen sample will be needed and this will be at about the same time as your partner’s egg collection.
Men should not ejaculate for 2-5 days before producing this sample. The fertility nurse will instruct your partner when to produce your sample on the day of egg retrieval. On rare occasions a second semen sample may be needed so men should stay locally to allow time for the embryologist to check the sample. If men wish to leave the unit please leave a mobile number with the nurse or receptionist for us to contact you should the need arise.
After Egg Collection
You will be given a letter for your GP, which informs him/her of your treatment. We advise that you have a day or two off work, resting at home following the egg retrieval.
Step 5 – Fertilising the eggs and embryo development (embryo storage only)
IVF or ICSI?
We want to give you the best possible chance that the eggs will be fertilised. At the same time we do not want to carry out any unnecessary interventions. There are two ways to fertilise the egg. If the sperm count is normal, we put about 100,000 sperm with each egg. This is IVF. If the sperm count is of poorer quality, we put just one sperm directly into the egg. This is ICSI (intracytoplasmic sperm injection). ICSI is much more complicated, can sometimes damage the egg and costs more than IVF. For these reasons, we prefer to do IVF where possible.
Is there a difference between the fertilisation rate for IVF and ICSI?
Following both IVF and ICSI we expect to have successful fertilisation in about 7 out of 10 eggs (70%). In a small proportion of both IVF and ICSI, there is unexpectedly no fertilisation. If this occurs with IVF, we may recommend ICSI in any future treatment.
Is there a difference in the pregnancy rate and safety of IVF and ICSI?
There is no evidence that the pregnancy rates differ whether the eggs were fertilised by IVF or ICSI.
If you have an extremely poor sperm count, there is theoretically a very small risk that your infertility could be passed on to a male child. If appropriate, we will discuss this in more detail with you in the clinic.
How do we decide if you need IVF or ICSI?
The embryologist will advise you about whether you need IVF or ICSI. Initially we base this advice on the sperm test before treatment and your previous medical history. The final decision cannot be made until we have analysed the sperm sample given on the day of egg collection. The advice also depends on the number of eggs collected.
Sometimes the advice is very clear. A normal sperm sample indicates IVF and a poorer quality sample indicates ICSI. Analysing sperm samples is complicated and sometimes difficult to interpret. Furthermore, there is considerable daily variation in sperm counts. In the clinic we will recommend either IVF or ICSI based on the evidence at that time. We will let you know on the day of egg collection if our advice changes so that you can make a final decision.
What happens to the egg and sperm?
After insemination, the eggs and sperm will be left in an incubator overnight.
How do we prevent laboratory identification errors?
A rigorous system is in place to cross check your eggs, sperm and embryos against your name(s). You are assigned a separate compartment in the incubator that is labelled with your name(s). Each laboratory dish (containing eggs, sperm or embryos) that is used in your treatment is labelled with your name(s). This identification system is tracked by RFID tags that link your eggs, sperm and embryos and record all actions taken.
Failed fertilisation
Failure of fertilisation is unusual. Occasionally, this happens even when both sperm and eggs appear normal. If this happens, we will make you an appointment to see you for individual advice and to discuss further treatment options.
Embryo development
A fertilised egg is called an embryo. You will be called by a nurse or embryologist the day after egg collection to inform you how many eggs have fertilised to make embryos.
An embryologist will update you on your embryo development three days after egg collection and two days later to inform you if any of the embryos are suitable to freeze.
Stages of embryo development


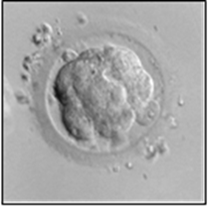

Embryo freezing
Not all embryos are suitable to freeze. There is a small risk that none of your embryos will be suitable to freeze. The embryologist will discuss the quality and the suitability of your embryos for freezing with you.
How does the embryologist decide which embryos are of good quality?
There is no absolute test that tells us whether or not an individual embryo can make a baby. The embryologist will look at the embryos and assess how quickly each embryo is dividing and whether all the cells are dividing evenly.
Freezing and thawing is stressful to the cells of an embryo. For some embryos all of the cells remain intact while in others all of the cells break up and are no longer viable. Only the best quality embryos are suitable for freezing. Poor quality embryos very rarely survive this thawing process. Thus we only recommend freezing good quality embryos.
What is the chance that a frozen embryo will make a baby?
We have analysed our results by looking at all the embryos that are frozen and subsequently thawed. If your embryos survive thawing and are transferred into your uterus, there is about a 30% chance of pregnancy.
There is no evidence that any babies resulting from thawed embryos have an increased risk of harm or abnormality.
What happens to the embryos is they are not frozen?
Embryos that are not suitable for freezing are put into a solution that stops them growing then they are discarded.
Your embryos will not be given to another couple.
Embryos may be donated to research or training but only with your written consent.
Use of gametes (eggs or sperm) in the event of death or mental incapacity
When eggs or embryos are stored we need to understand what to do with them in the event of your death or incapacity. The HFEA WT and MT forms outline the potential for posthumous storage and use on behalf of a NAMED partner. If you agree to use by your partner in these circumstances it is important to know what this means.
If you want your partner to have the option to use your eggs or embryos in the event of your death or mental incapacity, then you should complete the relevant section of the HFEA WT form on your online consent portal indicating your consent to storage of eggs and/or embryos and to the use of eggs or embryos in the event of your death or mental incapacity. This will then allow your partner to be able to make decisions about the use (or disposal) of your eggs or embryos made with your eggs if they are the named partner on the WT form and have provided their own sperm to create the embryos.
However, your partner could only use your stored eggs or embryos using a surrogate to carry a pregnancy. For this reason your declared intention on the HFEA WT form to allow your partner to use your eggs or embryos in the event of your death or mental incapacity needs to be validated to make that provision. The HFEA WT form does not provide the necessary consent for treatment of a surrogate. For your partner to take advantage of your declared consent for use of your eggs or embryos in the event of your death or incapacity you must also have signed consent for their use in treating a surrogate. In order to consent to this you must be seen by a counsellor to make sure you fully understand the implications of this and in order for a surrogate to use your eggs or embryos you must have undergone the relevant screening tests.
This package of work is not part of NHS commissioning for fertility treatment so you must pay these costs yourself. The approximate cost is £600 but is subject to change. Up to date costscan be viewed on our website or can be requested by emailing [email protected]
Some of the screening tests need to be completed each time you create embryos so there will be an additional charge of approximately £100 for each subsequent treatment cycle where you want to give your consent for use of your eggs or embryos in the event of your death or mental incapacity.
If you give your consent for use of your gametes or embryos in the event of your death but do not complete the necessary screening and counselling your consent will not be valid.
Please note that egg and/or embryo storage is not always clinically indicated so you may not have any eggs or embryos in storage after your treatment is complete.
Risks of treatment
Poor response
Sometimes despite our best efforts the ovaries respond very poorly or not at all to the FSH injections and a difficult decision has to be made about stopping the treatment cycle. Often this is not unexpected as you may have been warned that your ovarian reserve was low and that we were concerned that you would not respond to the injections. Sometimes however we are surprised when even with a predicted good response the ovaries do not behave as expected. We know that this is difficult and upsetting news to receive. Some women will have the opportunity to try again with an increased dose of FSH injections but for those women already on the maximum dose there is nothing more we can do to make the ovaries respond in a better way. If this happens to you we will explain the scan results in detail and talk about your options. We may ask you to go away and think about the advice we are giving then return to the outpatient clinic at a later date to discuss things further.
Ovarian Hyperstimulation Syndrome
A small number of women who are having treatment to stimulate the ovaries will develop a problem called “Ovarian Hyperstimulation Syndrome” (OHSS). Overall it affects only about 2% of women, but we will tell you if you are at higher risk – we may modify your treatment regimen accordingly. Detailed below are some specific answers to the questions you might ask.
What is ovarian hyperstimulation syndrome?
It is a combination of symptoms including enlargement of the ovaries, swelling and discomfort in the abdomen. Often it is associated with nausea and vomiting. Although we know that it is caused by the drugs we give you to simulate the ovaries, we do not know why only a small number of women develop these problems.
When will I start getting symptoms?
The usual time to start getting problems is a few days after the egg collection.
When will I get better?
The condition is self-limiting and will usually resolve completely within a couple of weeks of egg collection for egg storage most symptoms will be improving after a few days. We may ask you to attend for review if there are concerns about OHSS even though your treatment is complete.
What do I do if I feel unwell?
You may develop some of the symptoms described above and it may be difficult for you to know whether or not to be worried. If you are concerned at any time you should contact us directly (Tel: 0191 2138213). In particular we need to know if you are concerned about abdominal discomfort, start vomiting or are unable to drink anything.
Follow-up
We will confirm in writing how many eggs or embryos were stored. We might advise you to start the process again to increase the number of eggs or embryos stored. This might not be possible if you are storing eggs or embryos before starting urgent medical treatment such as chemotherapy.
We can always arrange follow up to discuss your treatment and future plans and of course are happy to answer any queries at that time. If you are going forward to other treatment e.g. chemotherapy we may agree to defer your appointment.
We will write to you on an annual basis about your stored eggs or embryos and to confirm that they are to remain in storage. We are happy to arrange an appointment to discuss this at any stage. If you think you would like to use the eggs or embryos for treatment we would need to see you in the clinic. We need a referral from your GP to make this arrangement.
Counselling Service
We are aware that undergoing fertility procedures is stressful and invades the most personal and private aspects of your life. Counselling can help to lessen your feelings of isolation and confusion, encourage you to recognise and understand your emotions and allow you to explore the options that you have available to make the decisions that are right for you.
We offer a counselling service that gives you the opportunity to talk to a sympathetic and impartial counsellor in a confidential setting. Each session usually lasts for one hour and further sessions may be arranged if necessary.
If you would like to see a counsellor please contact Barbara Hanson on 0191 2825503 or 0191 2829724 for an appointment.
Support Groups
Infertility Network UK
Email: [email protected]
Tel: – 0800 0087464 or 01424 732361
Donor Conception Network
Email: [email protected]
Tel – 020 7278 2608
Lily Foundation
http://www.thelilyfoundation.org.uk/
Email: [email protected]
Tel – 0300 400 1234 (Local Rate)
Daisy Network (Premature Menopause Support Group)
www.daisynetwork.org.uk/
Email membership&[email protected]
Macmillan (Preserving fertility)
Contacting the team
If you have any questions or concerns throughout your treatment the nurses can be contacted on 0191 2138213 option 1. Our telephone line is open 8am to 430pm Monday to Friday. Outside of these hours, there is an on call doctor available to speak to in emergencies only. The on call doctor is not able to change clinic appointments or to answer general queries that are not urgent. These types of calls must be made during clinic opening hours. We do our best to return your call as soon as possible but we are a very busy service so we may not always have someone available to speak with you immediately. At very busy times we have to triage the calls and prioritise the most urgent calls. This means that less urgent calls may take up to 48 hours for us to respond.
If you are leaving a message for us to return your call please take note of the following:
- State your full name and date of birth. It may be helpful to spell out unusual names.
- Remember to leave your telephone number. We cannot return your call if you do not leave your telephone number in your message.
- Speak slowly when stating your name and telephone number.
- Please do not leave multiple messages about the same issue. We will usually get back to you within 24 hours. If you have not heard from us within 48 hours of your first call please try again.
- If you are feeling unwell or bleeding in pregnancy and have not had a return call within 2 hours please call again. If you are experiencing a medical emergency and need emergency care please attend your local Emergency Department or ring 999.
Alternatively, you may wish to contact the nurses via email at [email protected] though we suggest that you only use the email address for non-urgent queries.
Patient feedback
We welcome your opinions and feedback on areas you feel have gone well or suggestions you may have to help us improve our service. If you have any problems during your treatment or are unhappy with the care you are receiving please contact the senior nurse (Sister Turnbull) on 0191 2138213. Fertility treatment is sometimes upsetting and frustrating particularly when things don’t go quite to plan or you don’t get the outcome you had hoped for. Sometimes having a chat with us will help relieve some of the tension and frustrations you may be feeling. We are always willing to listen.