Hundreds more people with an aggressive form of blood cancer can now be offered hope of a cure and “a new lease of life” from today thanks to an NHS drug rollout.
Glofitamab (Columvi®) will now be offered to around 300 people a year with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) — a form of non-Hodgkin lymphoma which has returned or not responded to chemotherapy — following approval by the National Institute for Health and Care Excellence today.
Faster treatment
This means people whose cancer has returned or not responded after just one previous course of treatment can now receive glofitamab faster – potentially avoiding gruelling rounds of treatment, with the drug previously only available to patients who had already undergone two types of treatment.
The drug given every three weeks via an intravenous infusion will be available from today thanks to the NHS fast-tracking access through its Cancer Drugs Fund, which provides patients with quicker access to the latest innovative cancer therapies.
Almost six in ten people with late-staged DLBCL saw their cancer go into complete remission after a course of glofitamab in combination with chemotherapy, during clinical trials.
Around 5,500 people are diagnosed with this cancer each year in England, which mainly affects men aged 65 and over, with the most common symptom being painless swellings of the glands.
“Forever grateful”
Clinical trial data shows that glofitamab, when given with chemotherapy, significantly increases survival and delays disease progression compared with a current standard treatment (R-GemOx)..
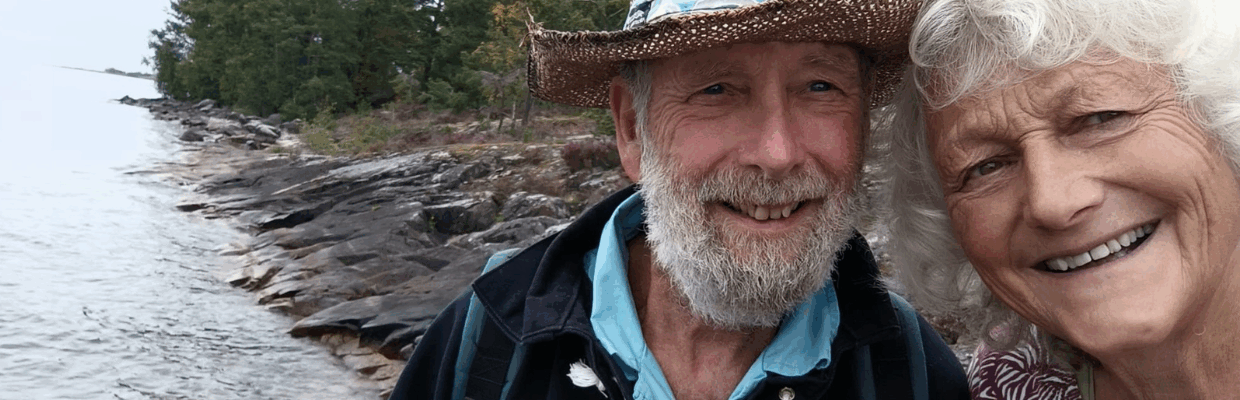
Chris Brown, 70, a retired inland waterways captain from Northumberland, was treated with glofitamab at Newcastle’s Northern Centre for Cancer Care following a diagnosis of stage 4 cancer.
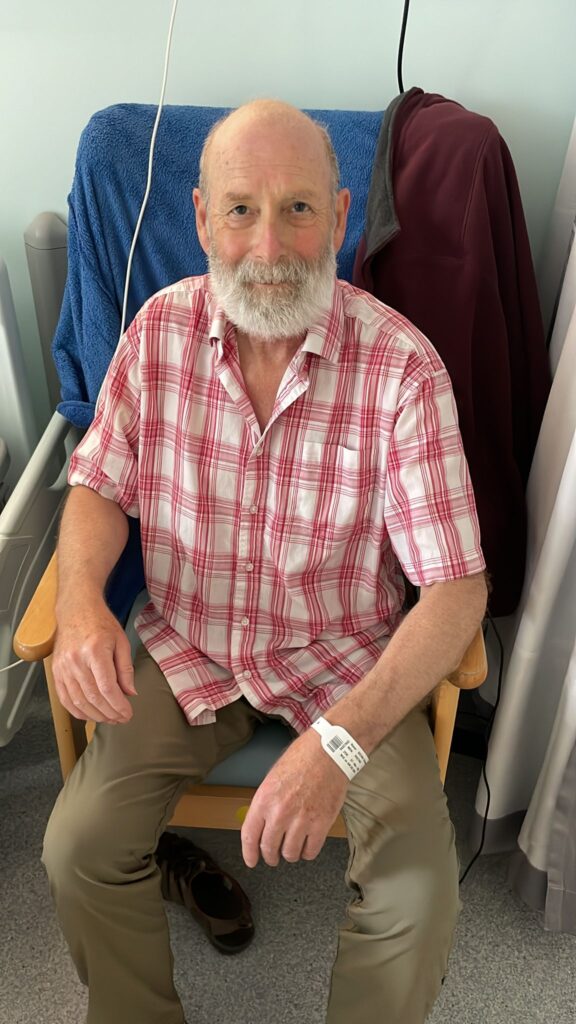
Chris, who has been in complete remission since February, said:
“I’ll be forever grateful to the NHS for giving me access to this treatment. The care I received at the Freeman Hospital in Newcastle was exceptional, and I was genuinely stunned by how effective the treatment was.
“I never imagined I’d hear the words ‘complete remission’ after a stage 4 diagnosis, but in February that’s exactly what I was told. It gave me a new lease of life – I’ve been able to enjoy things I thought were lost to me, like spending the summer boating with my family in Sweden.
“I am so pleased to hear that the glofit treatment is going to be available for people after only one previous treatment. Congratulations to all involved in bringing this wonderful course of treatment to the NHS. More developments can only improve our lives and hopefully reduce the anguish that families undergo when confronted with these diseases”.
Vital part of NHS cancer care
Dr Wendy Osborne, a consultant haematologist at Newcastle Hospitals who is part of the team who treated Chris, said:

“The availability of glofitamab has made such a huge difference for many patients, like Chris, and I’m so pleased that it will now be available to hundreds more patients earlier in their cancer.
“I have patients alive now who would have sadly died from high grade lymphoma if treatments like this had not been fast tracked by the Cancer Drugs Fund – it is such a vital part of the NHS’s cancer care”.
Professor Peter Johnson, NHS England’s National Clinical Director for Cancer, said: “Antibodies such as glofitamab that harness the power of the immune system to target lymphoma, are transforming the way people are treated and helping to boost the number of people cured.
“This is excellent news for patients with this aggressive form of blood cancer, with the NHS fast-tracking this cutting-edge treatment so that more people can benefit.
“It’s already changing lives, with people like Chris able to enjoy more precious time with their families”.
Pia Ballschmieter, Ph.D., UK Haematology Lead, Roche Products Limited said: “We are delighted by the National Institute for Health and Care Excellence’s positive guidance for Columvi-GemOx as a new second-line treatment for adult patients with relapsed or refractory DLBCL who are ineligible for autologous stem cell transplant. This decision is a significant milestone, providing a much-needed option for progressed patients in England and Wales. We are committed to making this treatment available across the rest of the UK as quickly as possible.”
Further information about the Cancer Drugs Fund (CDF)
- The CDF, which opened in its current form in July 2016, is used by NHS England to provide fast-tracked access for patients to all new cancer treatments approved by the National Institute for Health and Care Excellence.
- The CDF also enables access to promising new treatments that need more real-world data before a long-term NHS decision is made – this is called managed access.
- The CDF is now helping around 1,000 patients every month to access new treatments faster, with more than 108,000 patients accessing the latest cancer medicines on the NHS since its introduction in July 2016.
- Over 300 cancer treatment approvals have been fast-tracked via the CDF, with 50 new options added in the past 18 months alone.