On this page
We started a programme of change in 2024 to respond to current and future challenges in the organisation and the wider NHS, so we have a clear focus on rebuilding our services to make them stronger and sustainable for the future, with good outcomes.
At the heart of this is our patients. We want them to receive high-quality, safe care. Equally we want everyone who works here to feel supported and valued. We want staff to have the confidence to speak up about any issues or concerns – and know that we will listen and act, emphasising the opportunity to learn from improvement.
The demands on our staff and on the NHS are high, and we are all working hard. Our quality improvement approach ‘improving together’ isn’t about doing more. It’s about getting the fundamentals of care right and doing things differently.
With new executive leadership, refreshed Board and a new clinically led operating model, we have embarked on an extensive improvement journey to regain our previous high standards.
After twice being rated ‘outstanding’ by the Care Quality Commission in 2016 and 2019, the trust has experienced a number of difficulties in recent years with some serious concerns being raised. This culminated in a CQC rating of ‘Requires Improvement’ overall and ‘Inadequate’ for the well led domain in 2024. Throughout this time the care provided by our staff continue to be recognised as ‘good’ overall.
We have already made significant rapid improvements to our governance and approach to patient safety which has led to the removal of the license restrictions which had been imposed by the CQC.
Our programme of work, based on the CQC report and our own findings, has meant we’ve been able to make significant improvements in the specific areas of concern around governance, risk management, incident reporting and learning, culture, leadership and increasing the confidence of staff to raise issues, incidents and concerns.
We have a Board improvement plan in place and quality and safety priorities for each of our 8 clinical boards so we can measure and demonstrate the progress we are making with our continuous improvement journey.
We have also re-focussed our efforts on improving performance, significantly reducing the number of patients waiting long periods of time for their planned treatment or surgery, with more to do in diagnostics and cancer care.
We need to build on those foundations – through ongoing work with teams in our clinical boards and corporate services – to continue to progress.
CQC timeline
January 2024
- CQC report received with an overall rating of ‘requires improvement’.
- Official launch of ward accreditation programme in December 2024.
- Completion of Phase 1 action plan.
- Clinical Board improvement plans > move to quality and safety clinical board action plans.
- Development of corporate action plan > Phase 2 improvement plan.
- Conditions on trust license were removed in September 2024.
- Began rapid quality and safety peer review programme in September 2024.
- Number of focused visits including stocktake review by the value circle (TVC) in October 2024.
Performance
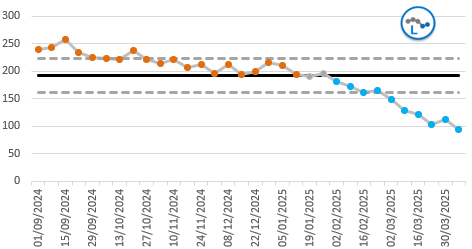
Our performance has improved significantly over the last year, but we have further to go to ensure that we shorten our cancer, diagnostic and emergency care waiting times in particular.
Diagnostic 6 week performance (04/24 – 04/25)
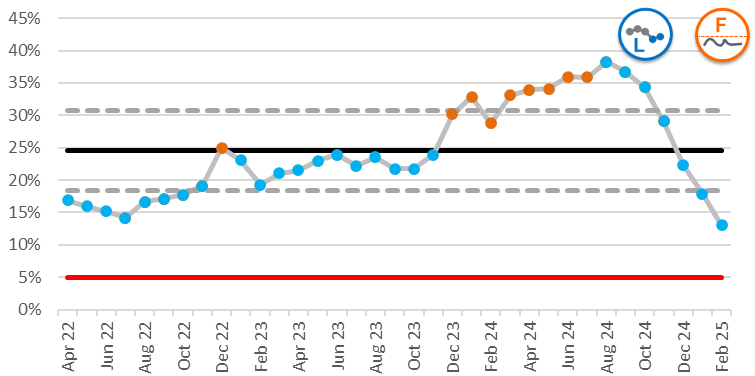
65 week waits (04/24 – 04/25)
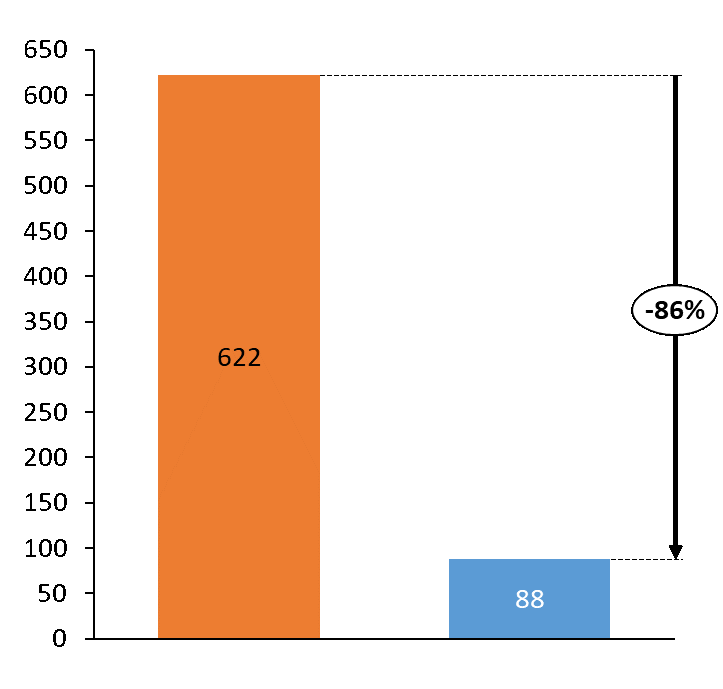
Over 62 day cancer backlog (04/24 – 04/25)
Our governance structure
A new governance structure has been embedded to support our improvement journey.
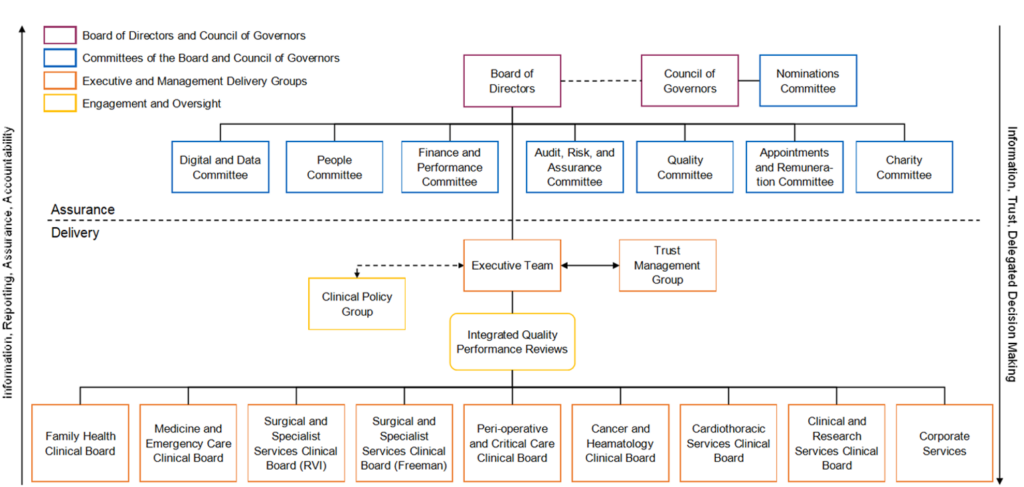
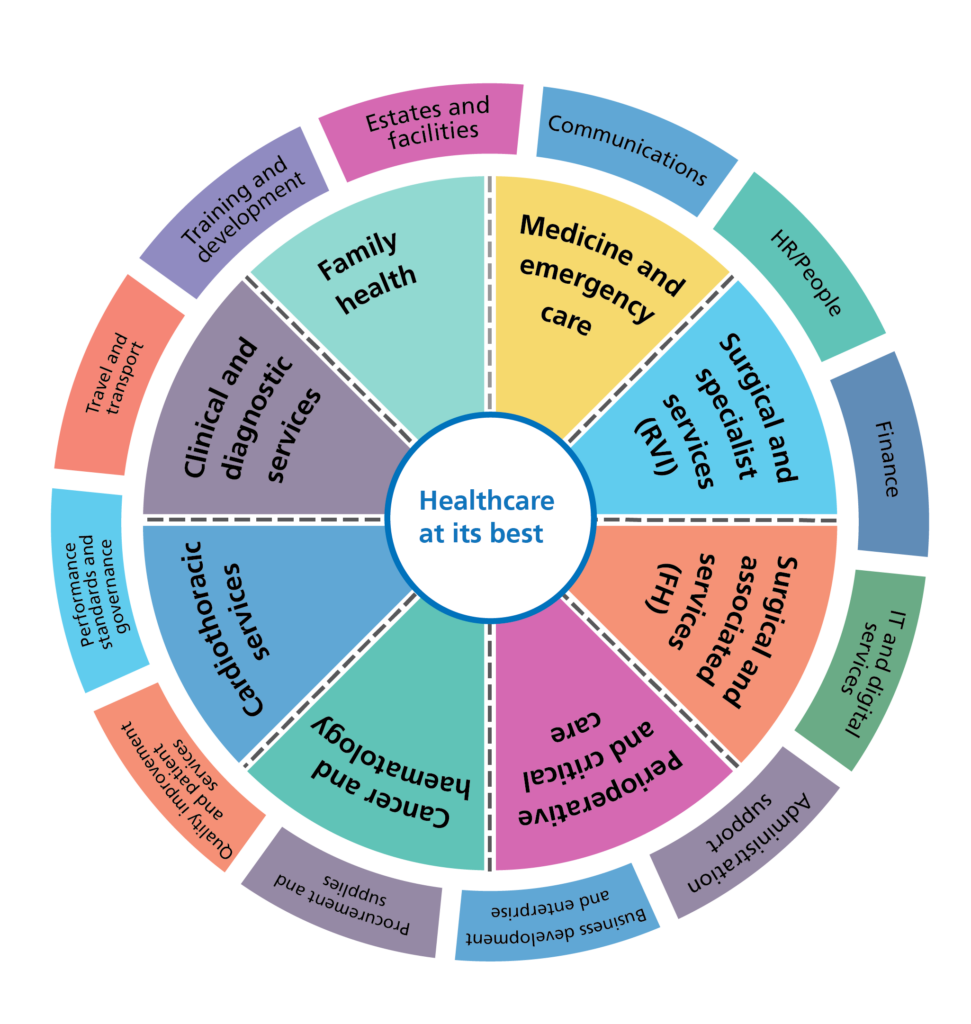
Our clinically led way of working
Leadership for our clinical services is structured and organised through 8 clinical boards.
Each board has responsibility for strategy, performance, workforce and finance in their area, covering a range of specialties and sub-specialities within directorates and is led by a triumvirate leadership team comprising of a clinical board chair, a director of operations and a head of nursing.
We also have a range of corporate teams and support services.